Commonly referred to as “getting your tubes tied”, tubal litigation is a form of permanent contraception well suited to women who are confident they don’t want to fall pregnant in the future.
What is tubal litigation?
Tubal litigation is a surgical procedure that provides permanent protection from pregnancy for woman. Other terms that are used to refer to tubal litigation include: permanent contraception, female sterilisation, and permanent birth control.
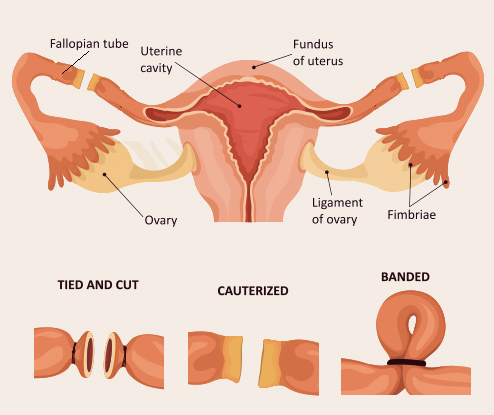
The procedure prevents the sperm from being able to reach the female eggs by either creating a blockage in the fallopian tube (through cutting, clipping, tying, or a combination of these). Another method is to remove the fallopian tubes entirely.
Why do women choose permanent contraception?
Permanent contraception is an alternative to other more common forms of contraceptives such the pill, implants, vaginal rings, intrauterine contraceptive devices (IUDs), and injections.
Unlike many of these other options listed, tubal litigation is not a form of hormonal contraception. This means it doesn’t come with the side effects that are often associated hormonal contraception, it doesn’t impact your menstrual cycle, and doesn’t affect your sex drive. It is also effective more than 99% of the time.
There is also a large body of research in the last decade that focusses on the use of tubal litigation to reduce risk of ovarian cancer. When this is a key consideration for the patient, I would generally recommend surgical removal of the tubes (bilateral salpingectomy) rather than tubal litigation.
Most women who undergo tubal litigation have already had children and feel their family is complete. There is also a growing community of Australian women who are childfree by choice who may elect to have their tubes tied. Either way, female sterilisation is an incredible serious and personal life choice. It is usually permanent and unlike male sterilisation (vasectomy) it is not a straightforward procedure.
How is the procedure performed?
There are three methods for female litigation: through laparoscopy, at the time of a C-section, or mini-laparotomy. Most gynaecologists will avoid the third option as recovery is longer and usually more painful.
In a laparoscopic sterilisation, small incisions are made to the abdomen, the abdomen is inflated with gas and then the operation is performed with the assistance of a medical telescope. This option is minimally invasive and considered a day surgery.
What do I need to know about female sterilisation?
- This procedure is generally permanent. Although a reversal procedure is available, its success is not guaranteed and the likelihood of falling pregnant is reduced compared to pre-tubal litigation.
- The procedure is not painless. It is also very normal to experience pain and nausea for up to eight hours after the procedure and ongoing pain and cramps for up to three days.
- There are risks and possible complications from the procedure including allergic reactions to the anaesthetic, damage to nearby organs, and infection or inflammation.
- As the procedure does not have any impact on the female menstrual cycle, periods will continue.
- Patients should avoid sex for a period after the procedure to allow for healing. If the procedure was done after childbirth, 4-6 weeks is commonly recommended.
- Female sterilisation does not protect against STIs.
If you’re considering a permanent form of contraception, it is important to consult a gynaecologist to ensure you’re fully informed. They should be able to advise you on what options are available to you, and how they suit your individual circumstances.
 Dr Joseph Jabbour is a gynaecology specialist who offers caring and professional medical advice for the diagnosis, management, and treatment of all kinds of female reproductive issues from cervical testing to minor gynaecological procedures.
Dr Joseph Jabbour is a gynaecology specialist who offers caring and professional medical advice for the diagnosis, management, and treatment of all kinds of female reproductive issues from cervical testing to minor gynaecological procedures.
He takes an evidence-based approach and is passionate about ensuring his patients are well-informed and empowered to make the best decisions for their health.